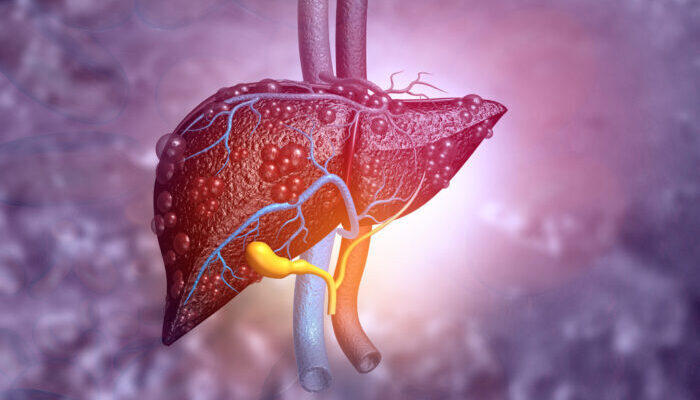
Non-alcoholic fatty liver disease (NAFLD) affects around 25% of the global population, being one of the most prevalent non-communicable diseases. NAFLD is defined by at least 5% macrovascular steatosis of the liver in the absence of any alternative etiology of hepatocellular injury, including excessive alcohol consumption. The spectrum of disease includes: (1) NAFL (non-alcoholic fatty liver) – macrovascular steatosis with or without mild inflammation; (2) NASH (non-alcoholic steatohepatitis) – NAFL with presence of inflammation and hepatocyte ballooning, with or without fibrosis; (3) Cirrhosis – characterized by chronic hepatic injury, extensive fibrosis and nodule formation; (4) Hepatocellular carcinoma – the most common primary malignancy of the liver, which can be present in the presence or absence of advanced fibrosis / cirrhosis. Due to its high prevalence, it is becoming the most common cause of liver-related mortality in all populations worldwide. Current standards of care for treatment of NAFLD encompass mostly lifestyle measures that are nonspecific and difficult for clinicians to ensure compliance. Although not all patients with NAFLD progress to more advanced disease, the high prevalence of NAFLD in the general population means the absolute number of “at risk” individuals is substantial and places a significant burden on the healthcare system. With development of non-invasive metrics of measuring fibrosis, there is an opportunity to identify patients with NAFLD, particularly those at risk of progression, prior to them progressing to stage 4 fibrosis / cirrhosis. Once a patient develops cirrhosis, their progression from compensated disease to decompensated disease with ascites, hepatic encephalopathy, variceal bleeding, hepatocellular carcinoma, or jaundice occurs at rate of 3-4% per year, which significantly decreases quality of life, increases hospital stays, and decreases life expectancy. As a result, NAFLD is currently viewed as a heterogenous disease with varying rates of disease progression.
NAFLD is associated with multiple risk factors, including increased caloric intake, sedentary activity level, central body fat distribution, metabolic syndrome, type 2 diabetes, and obesity. Type 2 diabetes is most strongly associated with progression to advanced fibrosis with a greater than two-fold increased risk. Dyslipidemia / hypertriglyceridemia and hypertension are also associated with advanced fibrosis, although they are less strongly correlated. Older patients also have a higher prevalence of advanced fibrosis, indicating that prolonged exposure to metabolic dysfunction may increase risk of progression. Precision-based quantification of these predictors to further risk stratify patients would be useful in the management of NAFLD.
There is a need for establishment of multidisciplinary care pathways to risk stratify and manage the burgeoning volume of patients with NAFLD, particularly focusing on patients at risk of progression and those with established advanced fibrosis / cirrhosis. This can be achieved through the utilization of (1) serum-based fibrosis biomarkers (e.g. APRI (AST to platelet ratio index), FIB4 (Fibrosis-4), NFS (NAFLD fibrosis score)) and (2) non-invasive elastography techniques (e.g. VCTE (vibration controlled transient elastography), SWE (shear wave elastography) and MRE (magnetic resonance elastography)). Furthermore, such pathway would facilitate a multi-pronged, personalized management plan developed in concert by hepatologists, endocrinologists, dietitians, physical therapists and psychologists. Sociodemographic, clinical, nutritional, physical function and pharmaceutical data obtained through these multidisciplinary encounters can be effectively leveraged for further scientific discovery and precision-based assessment of fibrosis, risk of fibrosis progression and decompensation, as well as assessment of multidisciplinary therapeutic interventions. Future research is warranted to elucidate the predictors of disease progression in NAFLD to develop and guide interventions while the disease is reversible. More research is needed to capture the diversity of the population with NAFLD and identify sociodemographic, clinical, nutritional, anthropometric, and microbiome-related risk factors associated with risk for NASH (Non-Alcoholic Steatohepatitis) progression. Phenotyping patients would lead to more accurate prognostication, facilitate better monitoring to prevent decompensation, and allow for development of precision-based, personalized management plans.


Comments are closed